Nobody wants to talk about COVID-19 anymore — and understandably so. By many measures, Princeton, and the country as a whole, have succeeded in mitigating the pandemic. Since March 2022, weekly U.S. death tolls have remained much lower than their previous heights, even during seasonal surges. Updated vaccines continue to be highly effective against severe disease and death. In some ways, it may seem to make sense to treat the disease like a common cold.
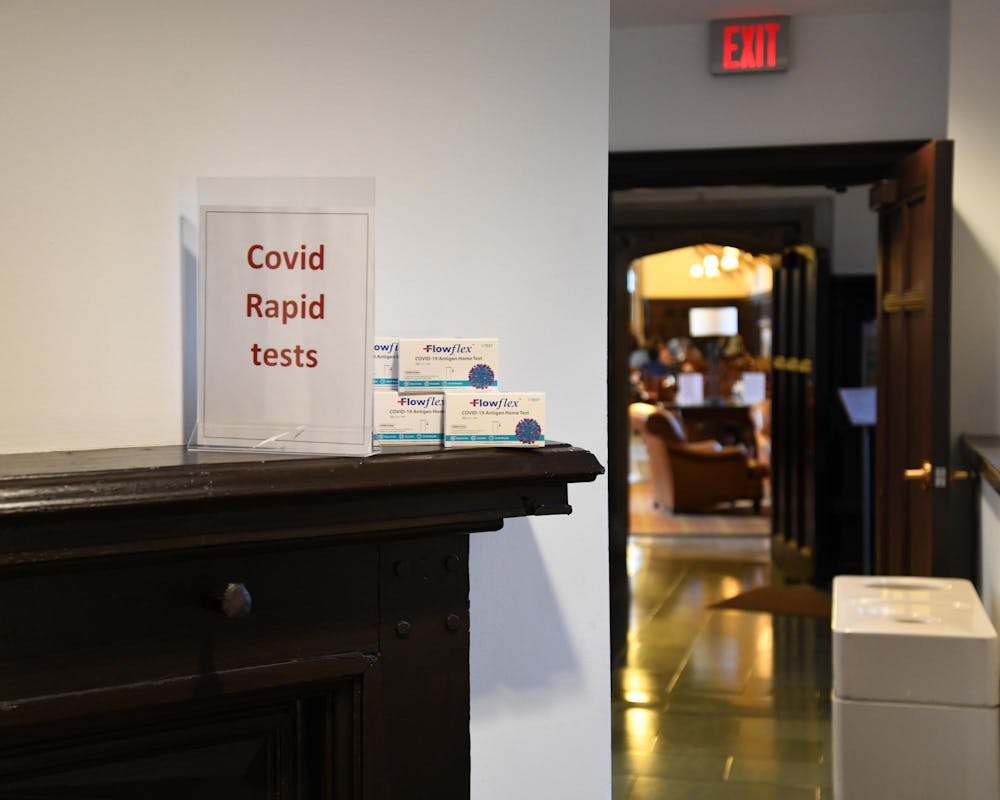
In fact, that’s exactly what Princeton’s current policy, in alignment with CDC guidelines, does. Students are no longer required to isolate when diagnosed with the disease, nor to report their positive tests or mask. Instead, “common-sense guidelines” are recommended “for all respiratory viruses,” and residential colleges no longer provide rapid antigen tests, just optional KN-95 masks.
However, in the face of continued concerns and unanswered questions about the health effects of COVID-19 reinfections, especially for disabled or immunocompromised individuals, it does not make sense to treat all respiratory viruses as equals. Princeton’s current protocols are not unique to — and therefore not appropriate for — addressing and mitigating the spread of COVID-19.
Though it does not make sense to return to pandemic-era restrictions like mandatory masking, Princeton must provide guidance for isolation and mitigation with best practices specific to COVID-19 in mind.
First, though a COVID-19 infection may be benign for most young people, the chance of severe disease is still much higher than that from the common cold. A recent study showed COVID-19, even with most of the population vaccinated or otherwise partially immune, remains 35 percent deadlier than the flu. In spite of this, the virus has evolved to be more contagious than it was in 2020. Together, these factors make for a virus that continues to present a unique danger to our health.
The threats posed by COVID-19 also transcend the initial infection — especially if one catches the virus multiple times. We’ve all heard about long COVID-19 — which most often causes long-term effects fatigue, headaches, lightheadedness, chest pain, and other issues. But some of the scariest effects of infection may be impossible to initially discern. A study published earlier this year shows that infection, even with a mild case of COVID-19, can lead to the equivalent of seven years of brain-aging. In adolescents in particular, this can often cause long-term trouble with memory and focus. Even confined to the lungs, the virus can trigger inflammation in the brain, causing lasting damage. Furthermore, the impact of COVID-19 worsens with repeat infections, even if those infections seem just as mild as the initial one.
Skepticism abounds about studies like these, given the mild nature of many COVID-19 infections. But given the sheer volume of literature showing similar results, we must take them seriously. It’s clear that the virus still poses a unique threat, and treating it as akin to other respiratory infections just doesn’t make sense. As we head into the winter season — and likely another on-campus surge — Princeton and the study body must recognize the continued danger of COVID-19, even if we don’t return to the policies of 2020 or 2021.
In fact, other campuses like Yale retain much clearer guidelines for how students and faculty should respond to a COVID-19 outbreak. In updated guidance for this fall, Yale’s Campus Health still requires that students who test positive isolate while they have a fever and wear masks for an additional five days in public. Yale also provides takeout meals rather than forcing infectious students to eat unmasked in the dining hall. These guidelines are clear and minimally invasive to student life while recognizing the unique threat COVID-19 continues to pose to people of all conditions.

Princeton also must offer clearer guidance as to what a student should do if their roommate tests positive for COVID-19, or vice versa. Yale makes it clear on their website that students who feel unsafe in their living situation can contact their residential college for additional lodging options. Princeton’s most recent advice—which is dated Fall 2023 and contradicts other current guidelines—also says students should find another place to sleep in their suite, or contact an email address that provides isolation help. However, it’s unclear whether this already amorphous policy is still in place given the lack of updates for the Fall 2024 semester. The University must make its policy on COVID-19 isolation among roommates clear to students as the virus continues to spread across campus.
Princeton’s current silence on this issue seems to suggest we do what many have already done in this situation: continue to live with your roommate, maybe mask up, and hope for the best. But as we head toward another winter season, this is not enough. Princeton should use its wealth of resources to offer temporary housing for any student who needs it for health concerns. As a March 2023 op-ed pointed out, the University must not place the burden on students alone to keep themselves safe.
Furthermore, the University’s silence on the continued spread of COVID-19 on-campus has arguably created a culture of apathy about it. While this may not bother those who do not have health issues or are willing to take risks, we must remain sensitive as a community about people’s boundaries. I’ve heard stories about students jokingly showing their positive COVID-19 test to a friend, unmasked. Behavior like this cannot continue. In making the necessary return to normal, we’ve forgotten the importance of respecting other people’s boundaries around health.
What this issue comes down to, then, is common sense. The term was rightly invoked late in the pandemic to rally support for loosening harsh restrictions amid a lower health risk. But perhaps we have gone too far in the other direction. COVID-19 is not the same thing as a cold or even the flu, and we must again use common sense to create policies — both at Princeton and elsewhere — which recognize that.

Shane McCauley is a first-year from Boston, who intends to major in one of the social sciences. He can be reached at sm8000[at]princeton.edu.